The power of case review
When things go wrong, we often talk to ourselves quite harshly. After an initial period of self-blame, a review of the particular case can be very healing.

Prof. Andreas Obermair
3
min read
•
Dec 1, 2024
Insights
Industry news
When things go wrong, we often talk to ourselves quite harshly. After an initial period of self-blame, a review of the particular case can be very healing.
I operated on a patient with a 15 cm left ovarian mass. She had a complicated surgical history including a previous ureteric injury elsewhere.
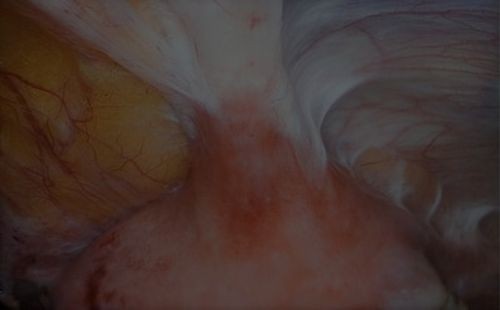
Intraoperatively, we managed severe omental adhesions. The mass was buried in bowel adhesions and I dissected the sigmoid colon of the mass, which took some time. I managed to enter the retroperitoneum, identify and trace down a double ureter on the left side. The mass was also stuck inferiorly where I had suboptimal access. Finally. I got the “thing” free from bowel.
10 days after surgery, I diagnosed a sigmoid colon leak. To say that I was not happy was an understatement. This complication was severe and I blamed myself for it. I was also concerned about how some of my colleagues would react.
One of my trusted colorectal colleagues took over her care and brought the procedure to a good end.
I was really not in a good space mentally for a couple of days. I want to share with you the steps I took to get myself back on track and also, some observations I made along the way.
First the steps:
I discussed the case with three colleagues including two colorectal surgeons.
I watched my video recording of this case a few times and finally also together with one of my colorectal surgical colleagues.
I checked my SurgicalPerformance outcomes.
I identified learning points.
I formally prepared a case review of this case.
Now to the observations and learnings garnered through the process of implementing the five steps.
Firstly, what I wanted to know most was how I would prevent this from happening in the future, if I were to operate on an identical case.
Hence, I discussed the case with another senior general surgeon who was not directly involved in the patient management. He was of the opinion that a leak test could have diagnosed this colon leak earlier.
Because I video record all my laparoscopic cases, I was able to watch the procedure a number of times. I can’t tell you how harrowing it is to watch a video of your own surgery where you KNOW it ends badly. By watching the video, I lived through the case again.
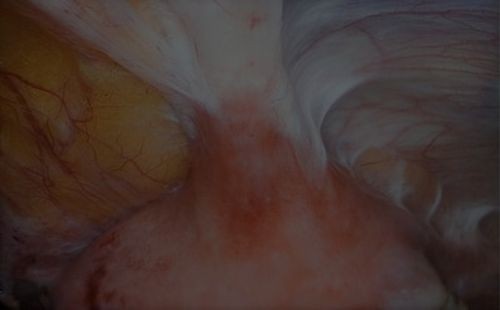
Initially, when I watched it on my own, there was nothing I would have done differently. Eventually, I did see a 5 second video snip that I suspected was the cause of the bowel injury.
I reviewed my video recording of the case with a trusted colorectal surgeon. He agreed that this 5 second part was where the injury occurred. “This is a thermal injury”, he said. “A leak test would have been likely negative.”
At around the same time, I was approached by a gynaecology colleague in the tearoom who at that time managed a patient who developed a ureteric fistula. “Are you OK?”, I asked him. I was puzzled because he seemed quite unfazed. Whereas I would have been equally devastated by a ureteric fistula as my sigmoid colon leak. The next day we were operating in theatres next to each other and I said “hello”. He then admitted that he had been faking it. He was, in fact, equally devastated and he felt that when I admitted that I was really bothered by my complication, it gave him permission to also grieve.
I checked my SurgicalPerformance outcomes and found that my most recent fistula (bladder/ureter/bowel) was several years ago and its overall incidence rate was way less than 1%. It gave me comfort to have certainty about my complication rates, instead of having to say “I can’t remember ever having had a complication like this”. If you can’t remember, it could be because your memory fails to remember events from many years ago, or because there was no complication. With SurgicalPerformance I don’t have to remember - I Know.
As part of 2024's CPD requirements, I will use this experience to prepare a Clinical Case Review. I recommend this activity not only to get CPD hours, but also as an opportunity to reflect... and to perfect.
All in all, his whole process of reliving the case, reviewing videos, developing learning points, writing and thinking was a very healing process that worked very well for me. The journey of learning and improving continues of course. But I must say that the more I reflect and learn, the more interesting and rewarding it gets.
When things go wrong, we often talk to ourselves quite harshly. After an initial period of self-blame, a review of the particular case can be very healing.
I operated on a patient with a 15 cm left ovarian mass. She had a complicated surgical history including a previous ureteric injury elsewhere.
Intraoperatively, we managed severe omental adhesions. The mass was buried in bowel adhesions and I dissected the sigmoid colon of the mass, which took some time. I managed to enter the retroperitoneum, identify and trace down a double ureter on the left side. The mass was also stuck inferiorly where I had suboptimal access. Finally. I got the “thing” free from bowel.
10 days after surgery, I diagnosed a sigmoid colon leak. To say that I was not happy was an understatement. This complication was severe and I blamed myself for it. I was also concerned about how some of my colleagues would react.
One of my trusted colorectal colleagues took over her care and brought the procedure to a good end.
I was really not in a good space mentally for a couple of days. I want to share with you the steps I took to get myself back on track and also, some observations I made along the way.
First the steps:
I discussed the case with three colleagues including two colorectal surgeons.
I watched my video recording of this case a few times and finally also together with one of my colorectal surgical colleagues.
I checked my SurgicalPerformance outcomes.
I identified learning points.
I formally prepared a case review of this case.
Now to the observations and learnings garnered through the process of implementing the five steps.
Firstly, what I wanted to know most was how I would prevent this from happening in the future, if I were to operate on an identical case.
Hence, I discussed the case with another senior general surgeon who was not directly involved in the patient management. He was of the opinion that a leak test could have diagnosed this colon leak earlier.
Because I video record all my laparoscopic cases, I was able to watch the procedure a number of times. I can’t tell you how harrowing it is to watch a video of your own surgery where you KNOW it ends badly. By watching the video, I lived through the case again.
Initially, when I watched it on my own, there was nothing I would have done differently. Eventually, I did see a 5 second video snip that I suspected was the cause of the bowel injury.
I reviewed my video recording of the case with a trusted colorectal surgeon. He agreed that this 5 second part was where the injury occurred. “This is a thermal injury”, he said. “A leak test would have been likely negative.”
At around the same time, I was approached by a gynaecology colleague in the tearoom who at that time managed a patient who developed a ureteric fistula. “Are you OK?”, I asked him. I was puzzled because he seemed quite unfazed. Whereas I would have been equally devastated by a ureteric fistula as my sigmoid colon leak. The next day we were operating in theatres next to each other and I said “hello”. He then admitted that he had been faking it. He was, in fact, equally devastated and he felt that when I admitted that I was really bothered by my complication, it gave him permission to also grieve.
I checked my SurgicalPerformance outcomes and found that my most recent fistula (bladder/ureter/bowel) was several years ago and its overall incidence rate was way less than 1%. It gave me comfort to have certainty about my complication rates, instead of having to say “I can’t remember ever having had a complication like this”. If you can’t remember, it could be because your memory fails to remember events from many years ago, or because there was no complication. With SurgicalPerformance I don’t have to remember - I Know.
As part of 2024's CPD requirements, I will use this experience to prepare a Clinical Case Review. I recommend this activity not only to get CPD hours, but also as an opportunity to reflect... and to perfect.
All in all, his whole process of reliving the case, reviewing videos, developing learning points, writing and thinking was a very healing process that worked very well for me. The journey of learning and improving continues of course. But I must say that the more I reflect and learn, the more interesting and rewarding it gets.


