A SurgicalPerformance tale on the impact of working with unfamiliar teams on surgical outcomes
It was one of those Monday mornings when I entered the operating room – “Good morning everybody!” The patient was still in the anesthetic bay, and our anaesthetist concentrated to place an epidural; the fellows were busy pulling up CT scan images and blood test results on the computer stations; and my scrub nurse’s focus was on her instrument count. I didn’t recognise her nor her scout.
Then the scout slowly turned to me and asked “By the way, what’s your glove size, doc?”. “Doc, this is our new Hasson cannula. Would you like to try it today?”
I did not know what to say. How would she not know my glove size? I’d operated in that hospital for many years. Had she not read my preference card? Had we not worked together before? Slowly, it began to dawn on me that, apart from my trainees, I recognised no one in “my theatre”. I wondered – “Am I in the right location?”
Here was “my” anaesthetist inserting an epidural, which I passionately try to avoid whenever possible. In one of the LACE papers, we have shown that epidurals are associated with a significantly higher incidence of postoperative “surgical” complications in pelvic surgery.
Here were “my” two scrub nurses I had never met before or worked with. One of them proudly shows me the new Hasson cannula. For the last 15 years, I have been an advocate for 5 mm ports and avoid any incision longer than 6 mm as much as possible (except for highly invasive cancer surgery).
I did not think this was a particularly good start of the day. When I later enter this case in SurgicalPerformance, I will rate the “familiarity of the team” for this case as a “1 – not familiar”. Should the surgery proceed? Or would the patient be better off delaying the operation and having surgery done with a better team, where all my team members are on the same page?
SurgicalPerformance and Working with Strangers
Flash forward to the present, and SurgicalPerformance has now collected data from more than 180,000 gynaecology surgery cases.
Recently, we analysed data on the impact of familiarity of the team on surgical complication rates. Would it have an impact on surgical outcomes?
In collaboration with Professor Robert Huckman from Harvard Business School, SurgicalPerformance introduced this data field a few years ago.
In his seminal article “The Hidden Benefits of Keeping Teams Intact” (Harvard Business Review October 2013), Huckman describes the impact of well-functioning and dysfunctional teams from various professions. I highly recommend reading it.
In the article, he describes an orthopaedic surgeon who performs 550 knee operations a year (2.5 times as many as the second most productive knee surgeon in that hospital) and completes the procedure in 20 minutes, compared to 60 to 120 minutes it takes for all other surgeons. This surgeon managed to secure a dedicated team of nurses and some of those nurses have worked with him for the last 18 years. His complication rates are comparably low.
Huckman provides another example from software engineering where a 50% increase in team familiarity was followed by a 19% decrease in defects, a 30% decrease in deviations from budget, etc.
However, no academic group has previously examined the association of familiarity of surgical teams with complication rates.
In my case, where I come to the operating theatre to meet obvious unfamiliarity – can we quantify the impact of unfamiliarity or even unfriendliness on patients’ outcomes (including complication rates)?
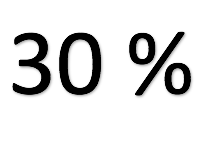
Data from SurgicalPerformance show that for major pelvic surgical procedures performed by unfamiliar surgical teams have a 30% higher complication rate compared to surgical cases performed by familiar surgical teams.
Surgical teams who are familiar with each other, where team members get on well with each other, where not every request needs to be verbalised but the nurse can anticipate the need of the surgeon, preparing for the next step without the need of a word said – these are well working teams. The Familiarity of the team is reflected in a significantly lower surgical complication rate.
Members of well-working teams know when and how to communicate; communication gets things done well and quickly.
Team members who know each other will know each other’s limits.
Team members who know each other respond easily to change; stress levels are much lower.
Do you often find yourself complaining that you are thrown into the operating theatre with unfamiliar team members you have to work with?
SurgicalPerformance allows you to capture your familiarity with your team.
- You then can quantify your team familiarity and compare it with your complication rates;
- You will also be able to compare your team familiarity in one hospital compared to another;
- You will also be able to compare your team familiarity with that of other surgeons.
With those quantified evidence, you could see your operating theatre manager to request change. Every case where you have to work with an unfamiliar team is a lost opportunity for them to save money.
If you have not done so already, I encourage you to take up a Premium subscription to SurgicalPerformance and start collecting data about how familiar you feel with your team – on a case-by-case basis.
Working with strangers is a huge lost opportunity not only to practice better medicine but also to do so at lower costs.