SurgicalPerformance is a surgeon-owned platform to generate insights on surgical and patient outcomes. This is important so that surgeons can feel safe – even when things don’t go to plan and complications develop.
Vaginal vault dehiscence after hysterectomy can be a serious complication because it can lead to a number of other complications, including vaginal and pelvic pain, vaginal discharge and bleeding and even complete separation of the vaginal incision leading to protrusion of the small or large bowel.
Early recognition and prompt treatment are important to minimise its impact and prevent further complications or sustained damage to the patient.
Is vaginal vault dehiscence a sign of poor quality surgery?
Vaginal dehiscence after hysterectomy can occur for various reasons and is not always a sign of poor quality surgery. Patient factors such as obesity, heavy smoking, immune system suppression; surgical technique, type of surgery (open vs laparoscopic), type of suture material used and postoperative activities can all contribute to the development of vaginal dehiscence. However, poor surgical technique or inadequate surgical training can increase the risk of vaginal dehiscence, and it’s important to consider all of the contributing factors when evaluating the cause of this complication. It is also worth noting that vaginal dehiscence is relatively rare and most women do not experience this complication after a hysterectomy.
While SurgicalPerformance provides feedback to our surgeon users, we sometimes analyse the incidence and risk factors of surgical complications; even if the incidence of a particular complication is low. We analyse de-identified data for all our learning and to share the insights we generated.
In this example, we pulled the data of almost 18,000 hysterectomies, which is one of the world’s largest data collections to date. In table 1 we show that 342 episodes of vaginal vault dehiscence, vaginal vault haematoma and pelvic infection were recorded from 17,994 cases, which gives an incidence rate of 1.9%.
Table 1
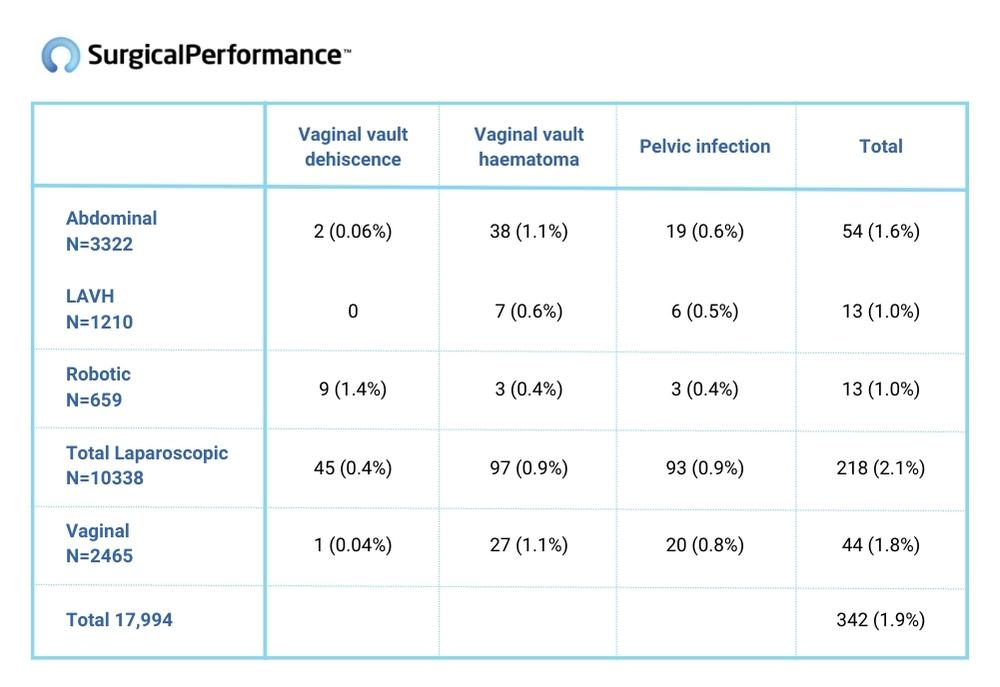
Interestingly, the incidence of vaginal vault dehiscence is statistically significantly more common after laparoscopic/robotic hysterectomy than with any other form of hysterectomy.
Despite the increased risk of vaginal vault dehiscence, minimally invasive hysterectomies (laparoscopic/robotic) still have numerous advantages over open, abdominal or vaginal hysterectomy types that outweigh by far the risk of a laparotomy. Numerous prospective randomised trials have shown that overall they are associated with less pain, quicker recovery time and an overall lower risk of postoperative complications compared to open surgery.
Can gynaecological surgeons minimise the risk of vaginal vault dehiscence?
To some extent, a surgeon can minimize the risk of vaginal vault dehiscence by following best practices in surgical technique and patient care. Some of the ways to minimize the risk of vaginal vault dehiscence include:
- Proper surgical technique: Using proper surgical technique, such as proper placement and tension of sutures, can help reduce the risk of vaginal vault dehiscence.
- Appropriate patient selection: Selecting patients who are less likely to develop complications, such as those who are not obese or heavy smokers, can minimise the risk of vaginal vault dehiscence. Patients at higher risk who need a hysterectomy despite belonging to a higher risk group, should be made aware of their elevated risks.
- Postoperative care: Advising patients to avoid heavy lifting and strenuous activity (e.g., promote the use of laxatives) and early pelvic floor exercise after surgery. Patients with lung issues could have their lung function optimised preoperatively to reduce the risk of a coughing fit.
- If a vaginal vault dehiscence develops, act swiftly: If bowel is visible, take the patient to the operating theatre straight away to close the vaginal vault, commence i.v. antibiotics and thereby minimise the risk of further infections. If you are uncertain, call a friendly colleague for advice. Document what and why you consider certain interventions and what you actually did.
It’s important to note that despite these precautions, vaginal vault dehiscence can still occur, but following these steps can help reduce the risk of this complication.