View our surgical video below.
It is unfortunate that the majority of ureteric injuries don’t get detected
intraoperatively. These injuries come to light sometimes up to 10 days post-surgery, many days after the patient has been discharged. Such delayed diagnoses cause major problems, often requiring several subsequent procedures to fix them.
I was once involved in a case where the patient required a nephrectomy several
months after a ureteric injury was diagnosed. The grief on the side of the patient and the heartache on the side of the surgeon is hardly describable. Cases like this often lead to formal complaints, payouts and sometimes litigation.
Being able to diagnose ureteric injury straight away intraoperatively, would result in the problem being a lot smaller. A urologist would come to theatre and either repair it or reimplant the ureter into the bladder. It’d still be bad and embarrassing, but a lot less than in a case of delayed diagnosis.
Ideally, we need a methodology that helps us avoid ureteric injury altogether.
Enter ICG!
I have been using ICG (IndoCyanine Green) for sentinel node biopsy in uterine and cervical cancer for several years. Recently, I started using ICG also to highlight ureters in extraordinary complex pelvic surgical cases.
I use ICG for my most challenging pelvic surgical cases where –
despite major efforts – I am unable to visualise the ureter.
My most recent case was an elderly woman with a BMI of 43 (she had thin legs),
with a previous hysterectomy plus four other previous pelvic procedures. She was on anticoagulation for AF. She had a right pelvic mass that bothered her and that had to be removed. Intraoperatively, and not unexpectedly, we found extensive adhesions involving loops of bowels and with a Trendelenburg positioning of 28 degrees, her bowels would not fall back as much as I would have liked. Patients like her, often also have some diverticular disease that makes the retroperitoneum even harder to dissect.
Normally, I would enter the retroperitoneum, identify and lateralise the ureter, secure the IP ligament and remove the mass through an endocatch bag. A quick procedure, you’d think.
I attempted to find the ureter… but couldn’t. I used all tricks that I acquired over the years, yet I still couldn’t see it. I felt uncomfortable securing the IP ligament and dissecting towards the pelvis without having been able to properly identify the ureter. After 45 minutes I gave up.
I discussed the case intraoperatively with my assistant and with my anaesthetist and prepared myself for a conversion to open surgery and all it’s terrible consequences given this patient’s central obesity.
The use of ICG saved my patient (and me) from converting her operation to a laparotomy and its awful consequences.
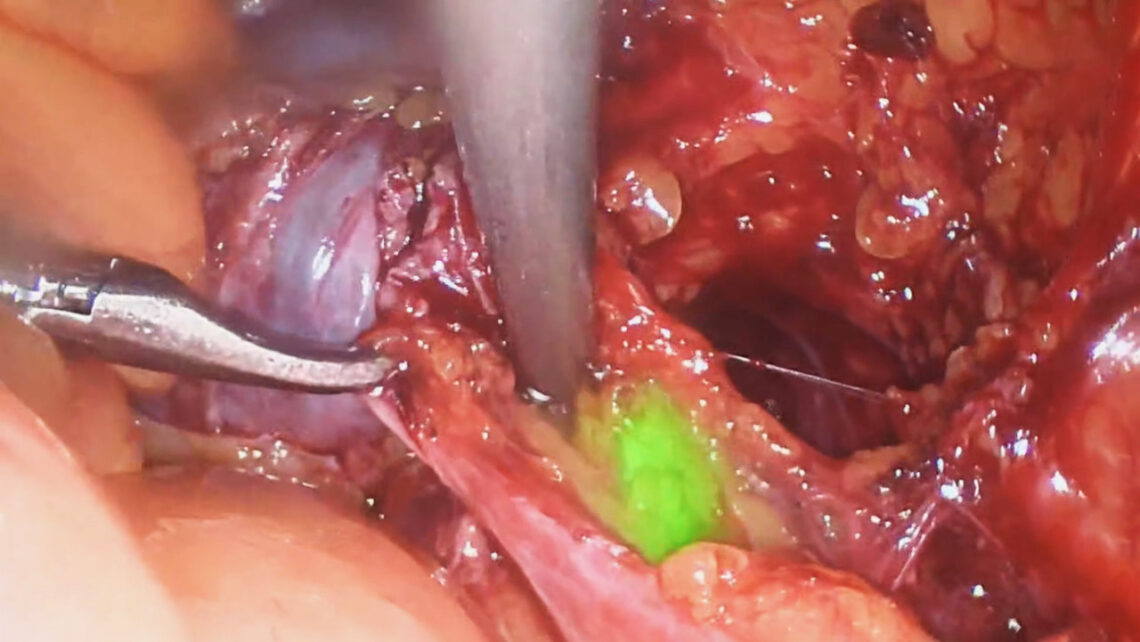
Suddenly, I remembered the ICG. I asked for a cystoscopy tray and a dose of ICG, injected a few ml of ICG in a retrograde way up the right ureter and re-laparoscoped her. Now, the ureter was beautifully displayed. It was not where I suspected it to be but much closer to the IP ligament. Now that I was able to visualise it, I was able to lateralise it and get it out of harm’s way. The procedure was completed super quickly within 10 minutes. The patient went home from hospital the following day. She recovered without problems.
Think of the incredible amount of pain and time using ICG saved the patient.. and me also!
I share this story because you likely also have this technology available to you. But you may not be aware that it’s like having a near-infrared system at your hospital. By applying this technique of injecting ICG into the ureter (or getting someone to do it), you will be able to visualise the ureter, avoid an injury and have a safer, happier patient.
From now onwards you can capture ICG use in SurgicalPerformance
From now onwards, SurgicalPerformance offers its users to document whether
retrograde ICG was used to highlight a ureter. It is available for all hysterectomies, adnexal surgical cases and for all endometriosis resection cases.
Highlight the ureter. Use SurgicalPerformance. Know Better!